How has MGH implemented artificial intelligence to benefit its patients?
Envision a world where diseases are predicted before they form or treatments are customized with the utmost accuracy. Mass General Hospital, one of the top five hospitals globally, is using AI to make this vision a reality. Their incorporation of AI includes increasing the accuracy in bipolar depression treatment, cancer prediction, and providing feedback to decrease obstetric risk.
In April of 2024, doctors Constance Lehman and Regina Barzilay introduced MIRAI, an AI model run on 128,000 mammograms (an x-ray on the breast area) to predict the chances of breast cancer in five years. The model exhibited an accuracy of 70% to 84%. Later, Barzilay and Dr. Sequist’s cancer team at MGH introduced the Sybil model; it was able to predict lung cancer with an 80% to 95% accuracy through examination of low-dose chest computed tomography (CT) scans before a human doctor was able to discern an issue. Barzilay says she is “excited about translational efforts led by the MGH team that are aiming to change outcomes for patients who would otherwise develop advanced disease” (3).
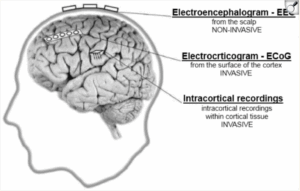
In addition to cancer prediction, MGH has been using a specific type of AI model, a large language model (LLM), to make decisions during the treatment of bipolar depression. The model is based on the upgraded version of GPT-4 (turbo). Currently, GPT-4 is the most advanced LLM in the world, which MGH has augmented by providing the restrictions for the appropriate treatment of bipolar depression prior to feeding a prompt to the model. The data was collected by providing the context and task, the knowledge for treatment, and the clinical vignette to make a decision on. The augmented LLM performed significantly better than the default LLM in the data: 51% to 23% optimal treatment in vignettes chosen respectively. As it stands currently, there is still work to be done, as there has been disagreement between clinicians and experts (2).
Another function of AI at MGH is decreasing obstetric risk. Obstetric risk measures the possibility of negative outcome during pregnancy or childbirth (4). Dr. Clapp, a fetal medicine specialist, and his team used natural language processing (NLP) to scan through vast amounts of data provided by the documents held at MGH on patients for delivery. The expected result is for the model to understand documentation, probabilities of a profile, and the outcome for a provided patient. The main goal, as stated by Dr. Clapp, is to “flag patients that require special care” so that the correct “risk level of maternal morbidity” is assigned (1). The biggest hurdle since 2023 to implementing the AI on real patients is getting approval from other clinicians and administrators, such as the FDA (1).
While there are many other ways that artificial intelligence is being incorporated at MGH, it is important to note that AI is an emerging technology that still requires further development and modification before being implemented. That being said, it is only a matter of years before AI starts saving lives with doctors and experts.
A visual of a humanoid-like robot interacting with an AI model https://www.kellton.com/kellton-tech-blog/how-ai-and-chatgpt-in-healthcare-elevating-the-game
Works Cited
- Using Artificial Intelligence to Decrease Obstetric Risk. (2023, February 21). Mass General Advances in Motion. https://advances.massgeneral.org/obgyn/article.aspx?id=1512
- Artificial Intelligence Decision Support Treating Bipolar Depression. (2024, May 15). Mass General Advances in Motion. https://advances.massgeneral.org/neuro/journal.aspx?id=2622
- AI for Early Detection of Cancer | Massachusetts General Hospital. (2024). Massachusetts General Hospital. https://www.massgeneral.org/cancer-center/news/ai-early-detection-cancer
- Andolsek KM. (2025). Obstetric risk assessment. Primary Care, 20(3).
- https://pubmed.ncbi.nlm.nih.gov/8378451/








Comments are closed.