The edge of sleeping and awake
Imagine waking up in the morning with an intense pressure on your chest. You see a dark figure across the room but can’t speak or move at all. Scary, right? Well, these are some of the symptoms of sleep paralysis, and it is much more common than you might think. But what exactly is sleep paralysis? What are its causes, symptoms, diagnosis, and treatment?
Sleep paralysis is the inability to move any part of the body, or the entire body, before falling asleep or when waking up. It doesn’t cause any harm to the person experiencing it; however, it can cause anxiety or fear. It typically occurs for a couple of minutes but can range from just seconds to around 20 minutes. The most common symptoms are the inability to move one’s legs or arms, inability to speak, drowsiness, hallucinations, and a feeling of suffocation or pressure on the chest. Those affected can be of any age, though it’s more common for people in their 20s or 30s. Studies show that sleep paralysis happens to about 30% of people at least once in their lives (1).
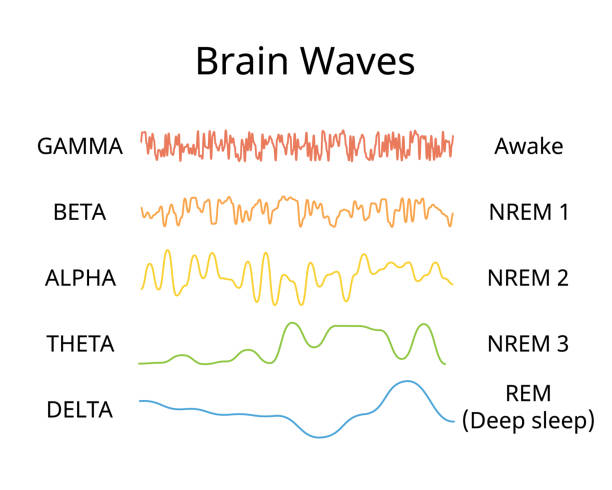
But how does sleep paralysis even happen? In order to understand that, it’s important to first know what hypnagogia is. Hypnagogia is the state between being awake and falling asleep. During hypnagogia, hallucinations of sound, movement, or illusions may occur. It’s very common, with around 70% of people going through hypnagogic hallucinations at least once in their lifetime. Hypnagogia happens when the brain’s electrical activity changes. In the brain, neurons communicate through five types of electrical waves. They are, from fastest to slowest, gamma waves, beta waves, alpha waves, theta waves, and delta waves. The electroencephalogram, also known as an EEG, is a machine that measures these signals. For reference, beta waves are produced more when awake along with some alpha waves, but when tired or drowsy, alpha waves are produced more. In the first stage of sleep, which is only a few minutes long, alpha waves are seen in less than 50% of the brain. Hypnagogia happens when the alpha waves in the brain decrease in this first stage of sleep (2).
If someone is still aware of their surroundings when going into the first stage of sleep, it can cause hypnagogic sleep paralysis, also known as predormital sleep paralysis: a type of sleep paralysis that happens during hypnagogia. The other type of sleep paralysis is the postdormital type; opposite to the predormital type, it describes when someone goes into sleep paralysis while waking up. In order to prevent someone from moving while dreaming during Rapid Eye Movement (REM) sleep, the body is temporarily paralyzed. If they wake up before the REM cycle is finished, they can experience hypnopompic—the opposite of hypnagogic—sleep paralysis (3).
There are many different causes of sleep paralysis. Some are from underlying conditions such as narcolepsy, insomnia, and substance use disorder. Other causes are mental illnesses, including bipolar disorder, PTSD, panic disorder, or anxiety. Finally, several causes are from day-to-day life, like certain sleep positions, a changing or irregular sleep schedule, medications, or stress.
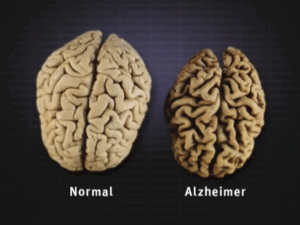
When diagnosing a patient a doctor may give them a physical exam or sleep evaluation. The doctor often asks questions about symptoms, sleep quality, medical history, mental health, occurrence frequency, and family history. A specific test they conduct is an overnight sleep study, also known as a polysomnogram, which is when a doctor watches someone while they’re sleeping to try and catch the sleep paralysis in action. Another specific test is the multiple sleep latency test, which is when a doctor measures sleep quality and how long it takes someone to fall asleep. It helps the doctor find out if the patient has narcolepsy, which is a neurological disorder that causes someone to be constantly tired during the day or to have sleep attacks (1).
There is no cure to stop sleep paralysis, but there are medications and ways to try and prevent it. The medications involve ones that help mental health or stop patients from reaching the REM stage while sleeping (1). One could also maintain a regular sleep schedule, have a bedtime routine, or try to reduce stress to prevent sleep paralysis. And while experiencing sleep paralysis, it’s important to stay calm, as it can reduce its duration. It’s also important to try to move small muscles to break through the paralysis, like the toes, fingers, or the tongue (3).
Although sleep paralysis may be scary and tough to experience, it’s overall harmless. If it ever happens to you, try your best to stay calm and make small movements. Be sure to have a good sleep schedule and take time for your mental health to prevent sleep paralysis from happening.
Sources
- (2021, November). Sleep Paralysis: What It Is, Causes, Symptoms & Treatment, Cleveland Clinic. https://my.clevelandclinic.org/health/diseases/21974-sleep-paralysis
- Yetman, D. (2020, October 26). What Is Hypnagogia, the State Between Wakefulness and Sleep? Healthline; Healthline Media. https://www.healthline.com/health/hypnagogia
- (2025). Sleep Paralysis, Aurora Health Care. https://www.aurorahealthcare.org/services/sleep-disorders/sleep-paralysis
Image




Comments are closed.