Components of CBT and Their Roles in Treating Insomnia
If you have had trouble falling or staying asleep for the past few days, there’s a good chance that you suffer from a common sleep disorder: insomnia. Most people are quite familiar with this illness; in fact, around 10% of the world population experience it. Insomnia may be a minor inconvenience, or a serious issue in one’s life (1). The body needs sufficient sleep to function at its best, which is where Cognitive Behavioral Therapy for Insomnia (CBT-I) comes into play. As one of the most effective treatments for insomnia, with around 70-80% of patients experiencing improvements (4), CBT-I has proven to be more effective than sleep medicine in the long term, elongate sleep time, and enhance the quality of sleep (3). So, what exactly is CBT-I and how does it work?
CBT-I treats insomnia through multiple therapeutic components and mainly targets the difficulty of starting or maintaining sleep. It follows a methodical approach where the success of this treatment depends on the therapist’s ability to foster the patient’s willingness to fully engage with the treatment process. A standard treatment would involve weekly sixty minute sessions over the course of eight weeks (2).
The specific components of CBT-I are split into two core components and two adjunctive components. The first of the two core components is Sleep Restriction Therapy (SRT). This component addresses sleep extension, which is a tendency to spend extra time lying awake in bed in an attempt to “catch up” on lost sleep (2). SRT works by first tracking sleep through a diary to calculate average sleep duration, and then setting up a sleep window about equal to this amount. For example, a person who sleeps seven hours a night would limit their time in bed to seven and a half hours. A gentler alternative is sleep compression, recommended for elders, which reduces time in bed gradually instead of making a large cut right away (4).
Another core component of CBT-I is Stimulus Control Therapy (SCT), which aims to break the negative associations people with insomnia develop between the bed and wakefulness. Patients typically pair their bed with wakeful activities such as reading, watching TV, or lying awake (2). To address this, SCT works by redesignating the bedroom as a place of rest, limiting the bed to only sleep and sex. Other methods include getting out of bed if unable to sleep within fifteen minutes and avoiding daytime naps. By associating the bed with sleep rather than wakefulness, SCT helps restore a positive sleep environment and sleep quality (4).
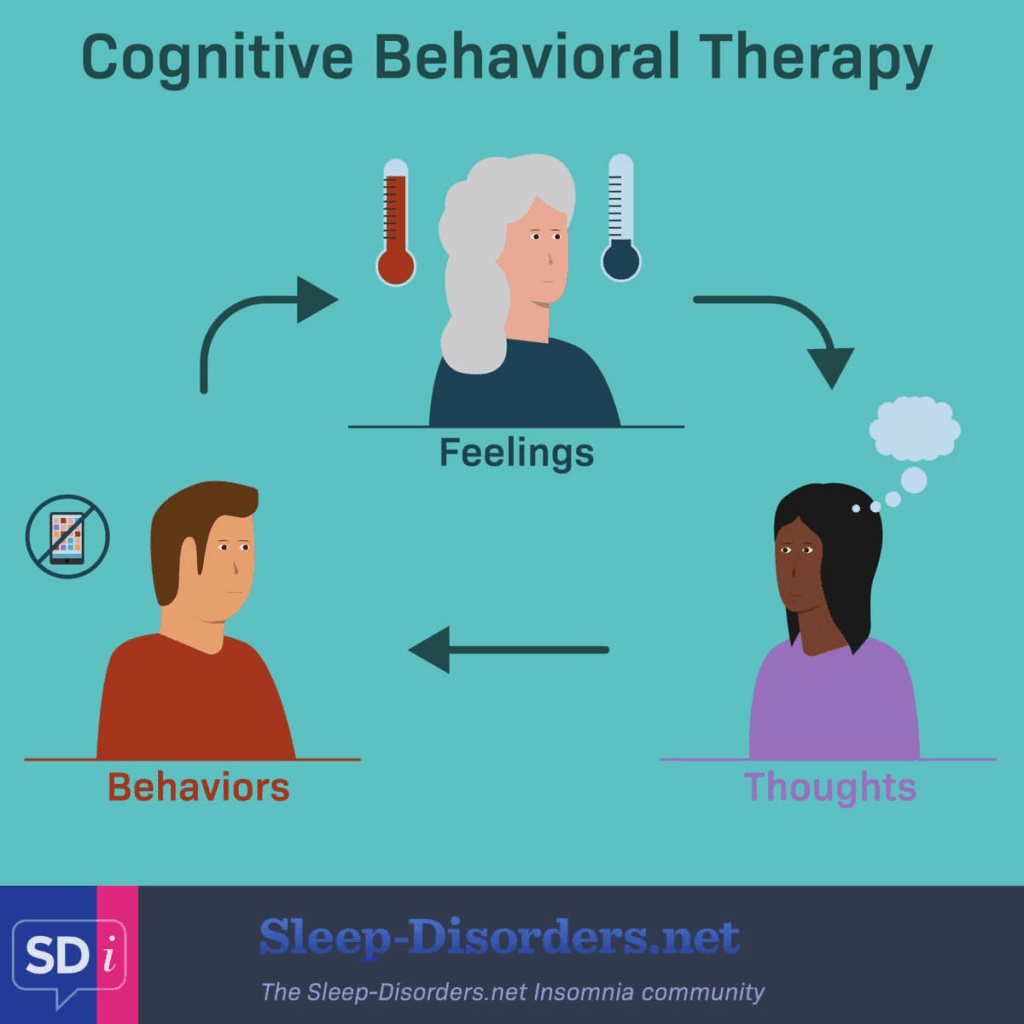
The Basic Workings of Cognitive Behavioral Therapies
Sleep Hygiene (SH) is one of the two adjunctive components of CBT-I. It focuses on educating patients about lifestyle and environmental factors that affect their sleep, typically involving strategies such as limiting caffeine and alcohol before bedtime, maintaining a comfortable sleep environment, and exercising on a regular basis. SH produces minimal results when used alone, but it remains a necessary component of CBT-I (2).
The second adjunctive component is Cognitive Therapy (CT), mainly helping to develop realistic sleep expectations. Therapists would work with patients to identify situations that promote maladjusted thoughts about sleep that stimulates insomnia, examine and challenge them through cognitive restructuring techniques, and finally replace them with better sleep-invoking thoughts. Patients could reduce anxiety about sleep and improve their sleep quality through CT strategies (2).
While sleep medicines provide simple and effective relieves for chronic insomnia, CBT-I remains a great option for overall long-term sleep length and quality without relying on medication. With the help of therapists and the four components of CBT-I, patients learn to restore their rightful sleep pattern and acquire a strong sleep routine, leading to more refreshing nights and better health.
Bibliography:
- for, O. (2023, August 18). Insomnia: What It Is, Causes, Symptoms & Treatment. Cleveland Clinic. https://my.clevelandclinic.org/health/diseases/12119-insomnia
- Walker, J., Muench, A., Perlis, M. L., & Vargas, I. (2022). Cognitive Behavioral Therapy for Insomnia (CBT-I): A Primer. Clinical Psychology and Special Education, 11(2), 123–137. https://pmc.ncbi.nlm.nih.gov/articles/PMC10002474/
- Understanding Cognitive Behavioral Therapy for Insomnia (CBT-I) | Veterans Affairs. (2023). Va.gov. https://www.veteranshealthlibrary.va.gov/142,41434_VA
- Cognitive Behavioral Therapy for Insomnia (CBT-I): An Overview. (2020, September 15). Sleep Foundation. https://www.sleepfoundation.org/insomnia/treatment/cognitive-behavioral-therapy-insomnia
Images:
- Cognitive Behavioral Therapy for Insomnia (CBT-I). (2020). Insomnia.Sleep-Disorders.net. https://insomnia.sleep-disorders.net/cbt
- Bed, I. (2023, September 14). A woman lies in bed and cannot fall asleep. Mental disorder concept,… IStock. https://www.istockphoto.com/vector/a-woman-lies-in-bed-and-cannot-fall-asleep-mental-disorder-concept-depression-gm1680182911-536605009




Comments are closed.