Scientists are getting closer and closer to a solution to HIV/AIDS.
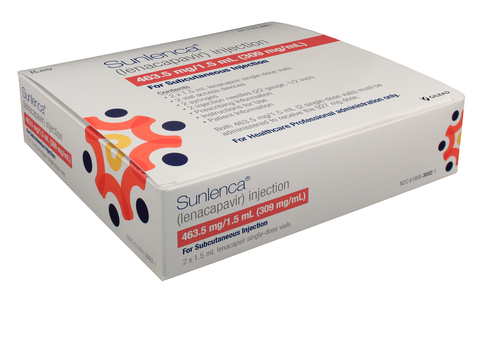
“It has been a challenge in the field to have simple treatment for this type of patient, so the approval of Lenacapavir is something we should be very proud of,” states Dr. Onyema Ogbuagu (the head of the Yale Antivirals and Vaccines Research Program). He is referring to Lenacapavir, the new milestone that scientists have reached in their efforts to cure HIV/AIDS (1). Recently, the United States Food and Drug Administration approved Lenacapavir, widely known as Sunlenca, to be prescribed to HIV/AIDS patients over the age of 18 (2). The drug’s main purpose currently is to treat those with the disease, but through comparison with other pre-exposure prophylaxis drugs on the market, scientists are simultaneously developing it to prevent those without HIV/AIDS from catching it (3).
Sunlenca, brand of lenacapavir.
Lenacapavir gives hope to many patients, as it is expected to seriously improve the quality of life for those diagnosed with HIV. The drug is classified as a capsid inhibitor and it is intended for patients undergoing antiretroviral treatment for HIV-1, but whose bodies are either rejecting current medication or experiencing side effects that jeopardize their health (4). But to what extent is this medication actually effective?
This drug was thoroughly tested and yielded fairly positive results in a study conducted by Gilead Sciences. The first portion of this study aimed to measure the effects of Lenacapavir on cisgender women. A total of 5,368 participants between the ages of 16 and 25 were gathered, specifically women from South Africa and Uganda. They were split into three groups and administered GS-6207 (Lenacapavir), Descovy (F/TAF), and Truvada (F/TDF)—two other existing HIV-preventative medications on the market (5). The Lenacapavir group exhibited no symptoms of HIV infection with a 100% efficacy rate (6).
The chemical composition of lenacapavir.
https://pubchem.ncbi.nlm.nih.gov/compound/Lenacapavir
The second portion of this study focused on Lenacapavir’s effect on transgender men and women, cisgender men, and gender non-binary individuals. In the study’s methodology, 3,265 patients were randomly administered (in a 2:1 ratio) two separate forms of treatment. While one group received oral doses of emtricitabine-tenofovir disoproxil fumarate daily, the other was vaccinated every 26 weeks with Lenacapavir injections under the skin. As a result, only 2 out of those given Lenacapavir developed HIV infections, whereas 9 of the participants that were previously given F/TDF yielded the same results (7). Based on these findings, it is reasonable to conclude that the new medication Lenacapavir is more effective than other HIV/AIDS preventative drugs on the market.
However, there are specific guidelines that come with taking such a medication. Lenacapavir is only provided by healthcare professionals and cannot be purchased as an over-the-counter drug. There are also multiple ways of taking the treatment, either in 300 mg tablets or through injecting 463.5 mg single-dose vials of Lenacapavir subcutaneously. Initiation dosing usually requires both and is followed by two injections every six months (2). Despite these details, the discovery of Lenacapavir is transforming HIV/AIDS treatment and saving the lives of many, a feat that would have been impossible without the hard work of the medical community.
Informational Bibliography
- Sofia Flores Rivera, V. (2023, August 30). Lenacapavir: Drug Offers New Hope for Multi-drug Resistant HIV. Yale School of Medicine. Retrieved January 21, 2025, from https://medicine.yale.edu/news-article/lenacapavir-drug-offers-new-hope-for-multi-drug-resistant-hiv/
- Clinicalinfo.HIV.gov. (2025, January 13). Drug Database: Lenacapavir. U.S. Department of Health and Human Services. Retrieved January 21, 2025, from https://clinicalinfo.hiv.gov/en/drugs/lenacapavir/patient
- Clinicalinfo.HIV.gov. (2024, November 19). Drug Database: Lenacapavir (HIV prevention). U.S. Department of Health and Human Services. Retrieved February 4, 2025, from https://clinicalinfo.hiv.gov/en/drugs/lenacapavir-hiv-prevention#:~:text=Lenacapavir%20is%20a%20drug%20that,for%20the%20treatment%20of%20HIV.&text=Lenacapavir%20is%20also%20being%20studied,drug%20to%20prevent%20HIV%20infection.&text=Lenacapavir%20belongs%20to%20a%20group%20of%20HIV%20drugs%20called%20capsid%20inhibitors..
- Prather, C., Lee, A., & Yen, C. (2023, December 5). Lenacapavir: A first-in-class capsid inhibitor for the treatment of highly treatment-resistant HIV. American Journal of Health-System Pharmacy. Retrieved January 21, 2025, from https://pubmed.ncbi.nlm.nih.gov/37767713/
- Gilead Sciences, Inc. (2024, September 19). Pre-Exposure Prophylaxis Study of Lenacapavir and Emtricitabine/Tenofovir Alafenamide in Adolescent Girls and Young Women at Risk of HIV Infection (PURPOSE 1). National Library of Medicine. Retrieved January 21, 2025, from https://clinicaltrials.gov/study/NCT04994509?tab=table#trial-contacts
- Full Efficacy and Safety Results for Gilead Investigational Twice-Yearly Lenacapavir for HIV Prevention Presented at AIDS 2024. (2024, July 24). Gilead Sciences, Inc. Retrieved January 21, 2025, from https://www.gilead.com/news/news-details/2024/full-efficacy-and-safety-results-for-gilead-investigational-twice-yearly-lenacapavir-for-hiv-prevention-presented-at-aids-2024
- Kelley, C. F., Acevedo-Quiñones, M., Agwu, A. L., Avihingsanon, A., Benson, P., Blumenthal, J., Brinson, C., Brites, C., Cahn, P., Cantos, V. D., Clark, J., Clement, M., Creticos, C., Crofoot, G., Diaz, R. S., Doblecki-Lewis, S., A. Gallardo-Cartagena, J., Gaur, A., Grinsztejn, B., … Ogbuagu, O. (2024, November 27). Twice-Yearly Lenacapavir for HIV Prevention in Men and Gender-Diverse Persons. New England Journal of Medicine. Retrieved January 21, 2025, from https://www.nejm.org/doi/full/10.1056/NEJMoa2411858




Comments are closed.