Researchers are searching every day for new breakthroughs in injection free diabetes control. Will they work?
Imagine waking up every day knowing that every meal, step, and moment that passes by carries the weight of a silent battle going on in your body. For over 830 million people worldwide, this situation is the reality of living with diabetes, a chronic disease caused by insulin deficiency (1). The most common method of treating diabetes is a daily—or several times a day—insulin injection. While these injections are helpful, they are physically and mentally taxing on patients, while also presenting many dangerous side-effects (5). However, as scientists are discovering day by day, there could be different ways to treat diabetes, including implantable devices (2), creating insulin producing cells from a person’s own stem cells (3), and orally taken insulin (4).
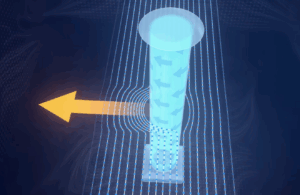
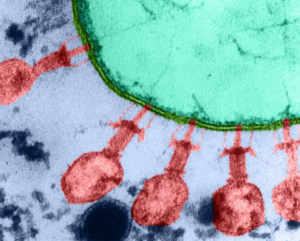
In 2023, engineers from MIT’s Department of Chemical Engineering made a breakthrough; an injectable device containing encapsulated cells that produce insulin could be the first step into injection-free diabetes control. Inside this miniscule device, there is an oxygen factory, which generates oxygen by splitting water vapor found in the body to keep the cells healthy. The tests run on this device so far have been mostly optimistic, including a test run on mice which kept their glucose levels stable for a month (2).
Implantable devices containing encapsulated cells and an oxygen factory.
Farther north, at the University of Alberta in Canada, scientists developed another alternative to insulin injections in 2023; the creation of insulin-producing pancreatic cells from a person’s own stem cells. Stem cells are unspecialized cells that have the ability to develop into specialized cells such as blood cells, muscle cells, and in this case, insulin-producing pancreatic cells. By taking stem cells from the blood and performing a process called “directed differentiation”—or chemically rewinding the cells back in time—they can be transformed into insulin-producing cells. Based on tests run by the Clinical Islet Program, the process of directed differentiation was able to reverse diabetes in the cells. While inserting insulin-producing cells sounds promising to the future of diabetes treatment, the transplantation has yet to be run on human cells (3).
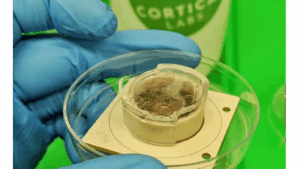
The final recent breakthrough against insulin injections is orally taken insulin. Researchers in the Li Lab at the University of British Columbia developed insulin drops that dissolve quickly when placed under the tongue. These drops contain a mixture of insulin and a “unique cell-penetrating peptide” sourced from fish byproducts. The peptide prevents the insulin from getting stuck inside the lining of the mouth and opens a pathway for it to effectively reach the bloodstream.
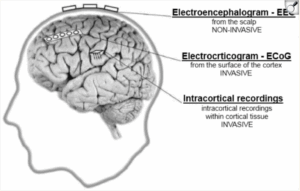
But why are so many alternatives to injectable insulin being developed? To start, the needles used for insulin injections pose many risks to patient health from cross contamination, needle pricks, accidental infections, and the exposure to not properly disposed needles (4). Additionally, insulin’s purpose is to lower the amount of glucose in a person’s blood level; when the dosage of insulin is too high, which can commonly happen in injectable insulin, a disease called hypoglycemia may spread. Hypoglycemia occurs when there are low glucose levels. Symptoms of this disease include dizziness, blurred vision, and disorientation. This disease is common in people who use insulin injections in their everyday lives (6).
Insulin pills developed by an MIT team.
In conclusion, the breakthroughs made so far, along with those occurring daily in the world of injection-free diabetes control, are beneficial to people who live with diabetes. Whether they prevent needle use or dangerous diseases such as hypoglycemia, these discoveries don’t only benefit people with diabetes, but also the future of science. For millions today, diabetes means a lifetime of needles. But with the daily emerging solutions, we can turn pain into progress and injections into memories.
Bibliography:
- Loke, A. (2024, November 14) Diabetes. World Health Organization.
Retrieved from
https://www.who.int/news-room/fact-sheets/detail/diabetes
- Trafton, A. (2023, September 18) An implantable device could enable injection- free control of diabetes. MIT News.
Retrieved from
https://news.mit.edu/2023/implantable-device-enable-injection-free-control-diabetes-0918
- Rutherford, G. (2023, November 6) New process produces purer, safer pancreas stem cells for potential transplant. University of Alberta
Retrieved from
https://www.ualberta.ca/en/folio/2023/11/new-process-produces-purer-safer-pancreas-stem-cells.html
- University of British Columbia. (2024, June 5). Oral insulin drops offer needle-free alternative for diabetes management. Medical Life Science News
Retrieved from
- Griffin, J. (2023, December 19). An implantable device could pave the way for continuous, injection-free diabetes treatment. National Institute of Biomedical Imaging and Bioengineering.
Retrieved from
- Lebovitz, H. (2011, April 22) Insulin: Potential Negative Consequences of Early Routine Use in Patients With Type 2 Diabetes. National Library of Medicine.
Retrieved from
https://pmc.ncbi.nlm.nih.gov/articles/PMC3632184
Images:
- Trafton, A. (2023, September 18) An implantable device could enable injection- free control of diabetes. MIT News.
Retrieved from
https://news.mit.edu/2023/implantable-device-enable-injection-free-control-diabetes-0918
- Trafton, A. (2019, February 7) New pill can deliver insulin. MIT News.
Retrieved from





Comments are closed.